Work Plan - 24/7 Access at Home
24/7 Access at Home Project (Quinte Sub-Region)Executive Sponsor: Wendy Parker, Executive Director, Brighton Quinte West Family Health Team
Team Lead: Mary Woodman
Current QI Advisor: Megan Jaquith
Background
The Ontario Palliative Care Network (OPCN), launched in 2016, is a partnership of community stakeholders including health service providers, health system planners, patients and their families. The OPCN is working with partners and the MOHLTC to transform palliative care in Ontario. This important work will help to address the gaps within the current system to ensure Ontarians have access to high quality palliative care.
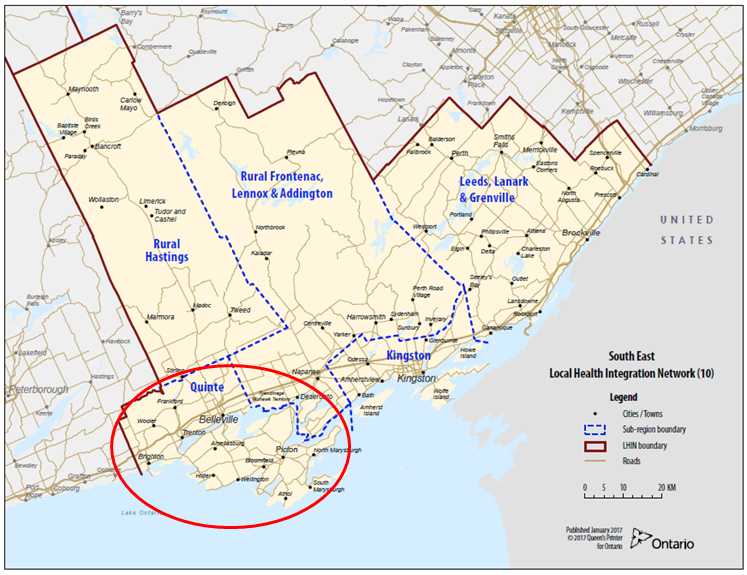
In the South East, the Regional Palliative Care Network (RPCN) acts as the principal regional advisor on high-quality hospice palliative care and is accountable to the OPCN. In consultation with various stakeholders, including health care providers and patient and family advisors in our region, five priority projects were identified, including “Improving Access to 24/7 Palliative Care at Home”.
The Quinte Health Link agreed to lead this project and a working group was established. The working group is comprised of members from Home and Community Care, primary care teams in Quinte, Paramedic services in Quinte-Hastings, QHC Nursing staff and regional family caregiver advisors. A quality improvement approach was taken to identify gaps in care, determine root causes, select areas of focus and then develop change ideas that would aim to improve outcomes for patients and their caregivers at end of life.
The working group members agreed to focus on changes that would aim to improve: Pain and Symptom Management at end of life; and Caregiver Support and Education.
A review of other jurisdictions experiencing similar challenges in palliative care led the group to explore a proven model of care in Nova Scotia. In 2016, Nova Scotia implemented “Paramedics Providing Palliative Care at Home” with excellent outcomes. In Nova Scotia, all Paramedics received LEAP training and acquired a new skill set which enabled them to take a palliative care approach and administer treatments that allowed the patients to remain in their homes 45% of the time. Their project outcomes demonstrated fewer transports for ER visits and admissions and allowed more patients to have their goals of care met.
Current State in South East
In Hastings and Prince Edward Counties, Paramedics currently respond to patients in their last 90 days of life an average of three (3) times and, by legislation, are required to transport these patients to a hospital emergency room (ER). Based on the Nova Scotia model, all front-line and supervisory Paramedics in Quinte, were trained through Pallium Canada in “LEAP for Paramedics”, with the training concluding on March 26, 2019. As an educational opportunity, LEAP training allows Paramedics to understand goals of care, symptom relief medications used in palliative care, the disease trajectory and how to have difficult conversations with patients and their families, among other things.
Currently, plans are underway to implement Phase 1 of this model of care in Prince Edward County in the summer of 2019. Leads from the working group, the Prince Edward Family Health Team (PEFHT) and Home and Community Care (HCC) are collaborating to develop processes and protocols required for this system change including how to identify patients and how to register patients in the program. Initially, patients receiving palliative care services from PEFHT and/ or HCC will be identified and approached with the intent to register them in the program. This will then allow 911 dispatchers to alert the paramedics that they will be attending a patient with known palliative care needs and whereby a solid plan of care is in place. The goal will be to respect the patient’s wishes and avoid transport from home to ER whenever possible. It is assumed, based on Nova Scotia’s experience that up to 50% of transports will be avoided and the remainder will still require an ER visit or hospital admission. Phase 2 is expected to be implemented across Belleville and Quinte West.
Provincial and National Landscape
This model of care is currently spreading across Canada (Canadian Foundation for Healthcare Improvement). CFHI is engaged with both the York and Ottawa projects as a funder. Their plan is to support information sharing from the CFHI projects and support spread and scale of innovations when available. The OPCN facilitated a provincial knowledge transfer and exchange webinar on March 8th, 2019. There are currently 11 sites in Ontario exploring this program, with South East as one of the first, having a large group of paramedics fully trained. However, there are still many discussions that need to take place at the provincial level regarding scope of practice and the Ambulance Act (1990) before this program can be fully implemented in Ontario. The Ontario Community Paramedicine Secretariat will take the lead in these decisions.
If you would like to learn more about the project please contact any of the following members of the working group or the RPCN Lead:
Mary Woodman: WoodmanM@bqwchc.com or Mike Slatter: SlatterM@hastingscounty.com
